Children's Hospital Los Angeles
Center for Endocrinology, Diabetes & Metabolism
The Sugar Ray Leonard Foundation is honored to support the Center for Endocrinology, Diabetes and Metabolism at Children’s Hospital Los Angeles and their groundbreaking work in diabetes care and research.
As one of the largest endocrine programs in the country, the Center is pioneering pediatric care, clinical and basic research programs in all types of diabetes, as well as disorders of human growth, bone metabolism, thyroid issues and adrenal disease. The Center provides comprehensive, state-of-the-art, interdisciplinary care, education and training to nearly 1,800 children with type 1 and type 2 diabetes and more than 4,600 patients with other endocrine disorders each year.
Through our philanthropic support, we have collaborated on many important initiatives with the Center detailed below.
2018-2025 Highlights
Embedded Psychology Program
The EPP was established in July 2016 thanks to the CHLA Endocrinology Ambassadors—parents with children cared for by the Center for Endocrinology, Diabetes and Metabolism (CEDM) who recognized the importance of having a psychology service within the CEDM. Through the EPP, any patient—regardless of their ability to pay—may receive psychological support.
Since 2017, The Sugar Ray Leonard Foundation has helped support the Embedded Psychology Program in the CEDM. Currently, one psychologist, Cynthia Muñoz PhD, MPH, holds an appointment of 60% time as an embedded member of the CEDM team. Dr. Muñoz is available on-site in the Endocrinology clinic 3 days per week. Dr. Muñoz provides ongoing psychological services both in-person and via HIPAA-compliant telehealth platforms specifically for the Type 1 and Type 2 Diabetes Clinics, Congenital Adrenal Hyperplasia Clinic, Healthy Weight Clinic, and the Bariatric Surgery Program. In addition, she is available to coordinate care with other members of each patient’s health care team including both CHLA, USC, and community-based health care professionals. In her role, Dr. Muñoz continues to provide the following:
Introduce psychological support when care is first established with the CEDM. This allows families to create a trusting family-professional relationship that includes mental health professionals from the beginning. EPP psychologists are available to meet with families who are new to the CEDM within either the outpatient or inpatient setting. In this manner, the stigma of receiving support from a mental health professional is minimized and access for ongoing mental health support is maximized. This also allows EPP psychologists to address patient and family concerns proactively by providing strategies and resources before the concerns become major problems.
Conduct mental health screenings. Annual depression screenings are recommended by the ADA Standards of Care for all pediatric patients with diabetes. This includes the nearly 2,000 children with all types of diabetes who received care at CHLA. EPP psychologists are available to conduct these screenings and to provide critical follow-up support and resources in clinic at the CEDM and in collaboration with outside services in the community. Eight hundred and twenty-eight patients had depression screening completed last year, at times identifying significant depression that would have otherwise not been identified.
Provide ongoing support. Some patients benefit from ongoing outpatient psychological support. In addition to meeting with families during scheduled appointments with their medical team, the EPP psychologists are available to meet with patients and families on non-clinic days. This allows children and families to address treatment-related barriers, and it promotes the continuity of emotional support.
Collaborate with the CEDM team. Managing a chronic illness is complex. As members of the interdisciplinary CEDM team, EPP psychologists consult and collaborate with all CEDM team members—including providers, social workers, nurses, dieticians, financial analysts, schedulers—on an ongoing basis. This collaboration promotes optimal family-provider communication and informed decision-making for the provider team.
Provide referrals. EPP psychologists are available to provide families with referrals to the CHLA USC UCEDD and/or outside agencies for psychodiagnostic assessments, psychotherapy and psychiatric evaluations. When the need for a referral to other members of the CEDM team is identified, EPP psychologists efficiently communicate the patients’ needs with colleagues.
Serve as liaisons with community agencies. With consent, EPP psychologists coordinate care with educators and community personnel to promote seamless care for each patient. EPP psychologists are available to collaborate with schools, but also with sports teams, afterschool activity programs and community-based therapists.
With thanks to funding from the Sugar Ray Leonard Foundation, Dr. Muñoz and her team, Dr. Chao and Nancy Chang are able to continue their work for children and families living with diabetes.
Type 2 Clinic
Type 2 diabetes (T2D) is a public health crisis affecting children and adolescents throughout the country, disproportionately impacting Americans of ethnic and racial minorities and those from disadvantaged backgrounds.
Children and adolescents with the condition face a future of serious diabetes-related complications that often appear early and can shorten a child’s life span.
Research shows that patients who develop T2D during childhood experience significantly higher rates of kidney disease, retinopathy, nerve damage and cardiovascular problems than those who acquire the disease in adulthood. If the prevalence of T2D continues to increase, the number of youth with the condition may increase more than fourfold, causing a tremendous burden to families and the overall health care system when patients fail to adhere to medical recommendations to control their diabetes.
The CHLA Type 2 Diabetes Clinic opened in January 2017 and is the first clinic in the nation dedicated to addressing the multifactorial issues faced by adolescents and young adults with T2D. The clinic focuses on empowering patients to manage their diabetes, while also addressing their weight management and psychosocial needs along with their personal, familial and environmental barriers to achieving good health.
Clinic Achievements in 2024
The number of patients CHLA treats for Type 2 diabetes has more than doubled since the pandemic, a national trend. At CHLA, this patient population is moving toward surpassing the number of patients they treat with Type 1 diabetes.
The clinic saw 961 patients with type 2 diabetes between 7/1/23 to 6/30/24, almost three times the number seen before 2019. Following up on an award from the American Diabetes Association in 2024, they piloted a team clinic for type 2 diabetes. A similar study has been ongoing for our patients with type 1 diabetes. This funding will allow the Hospital to evaluate whether group medical appointments are acceptable to families and provide important psychosocial benefits to middle and high schooler student with type 2 diabetes.
The Type 2 Diabetes clinicians and caregivers are dedicated to providing education about options for care while giving patients the opportunity to have a greater say in their treatment. Their staff of diabetes specialists, nurse practitioners, a psychologist, and social workers help young people become empowered to manage their care for life, while supporting their transition to adult healthcare. With the patient population served at CHLA and in all their clinics, their staff is mindful of the social determinants of health and issues of equity that influence the health of our patients and families.
Other Clinic Goals and Achievements
Aimed to increase patient motivation and provide patient-centered care by creating opportunities for individuals to participate and actively engage in their own diabetes management.
The “clinic compass” is a document developed to help patients identify their individual goals and facilitate communication between the patient and provider team, allowing the visit to be directed by the patient’s goals and not the provider’s goal.
Increased average clinic attendance per patient from 2.1 visits to 3.2 visits per year.
This more closely aligns with the American Diabetes Association Best Practice Guidelines, which recommend four visits per year.
Designed and implemented CLUB visits (Control your diabetes by Learning life skills and Understanding your Barriers) to address psychological barriers during the emotional adjustment period after patients receive a type 2 diabetes diagnosis and to direct the need for better treatment adherence.
CLUB visits are composed of four distinct sessions to help patients develop self-management techniques and practice coping skills in a supportive group environment. This semi-structured curriculum includes identifying sources of stress and stress management, working through issues of diabetes disclosure and managing peer relationships and anxieties in the school environment.
While the adolescents are involved in their activities, their parents participate in a separate group where they learn parenting skills and behaviors to support their child’s care at home. CLUB visits are mandatory sessions for patients with hemoglobin A1C (HbA1C) measurements greater than 8.0%. Between January 2017 and August 2019, 70 patients have participated in at least one CLUB session.
To implement a weight management program tailored for patients with type 2 diabetes, the clinic adapted the evidence-based Kid N Fitness© curriculum.
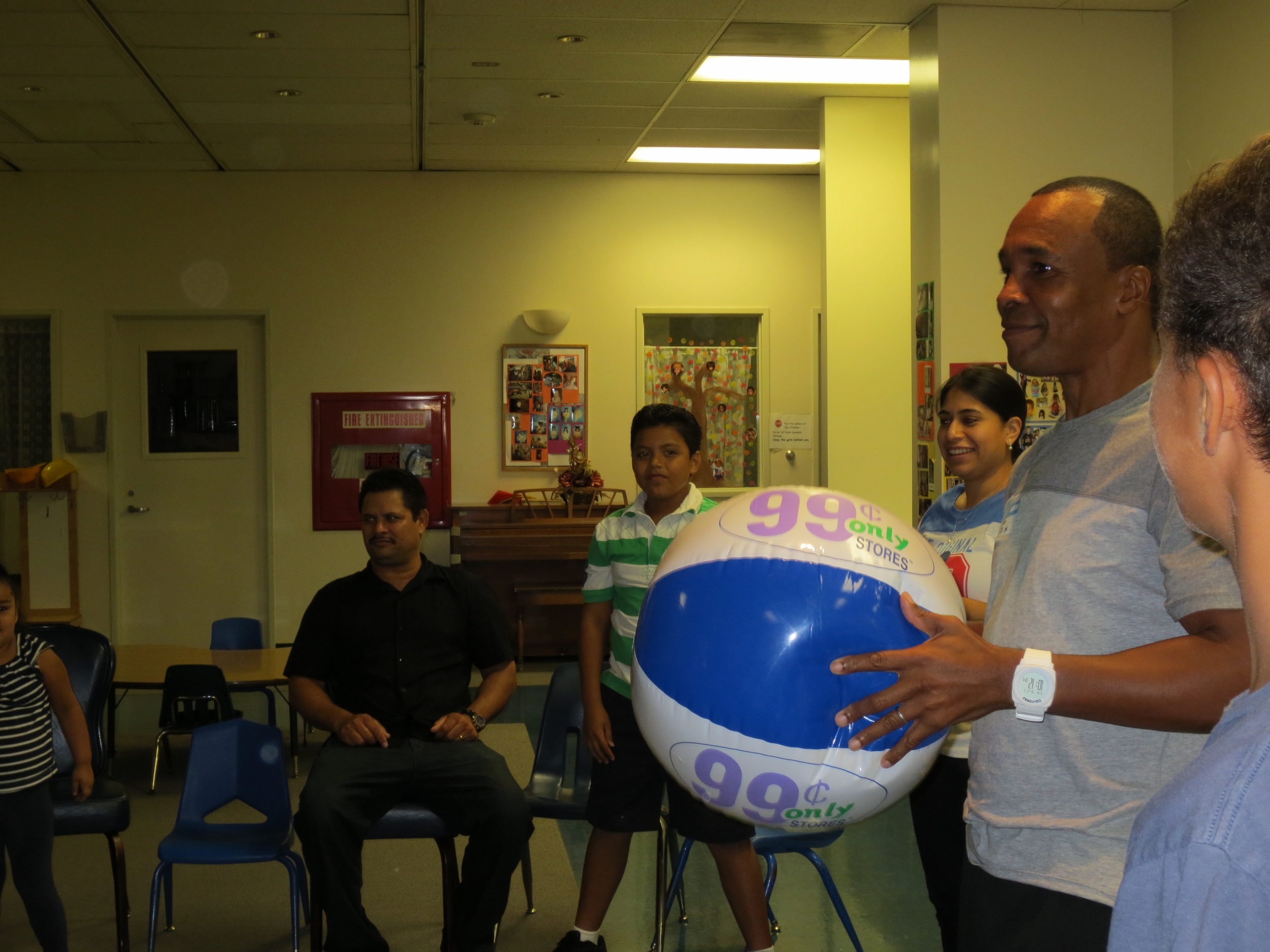
The family-centered group sessions are offered to families in their home neighborhoods through partnerships with the Weingart YMCA Wellness and Aquatic Center in South Los Angeles and with the Wellness Center at the Los Angeles County USC Medical Center. The program has six sessions that meet every other week. Since July 2017, nearly 58 families participated in various program sessions with 21 families completing the entire program. Participants experienced a greater improvement in BMI when compared to a control group of peers who did not participate. This is a very important finding because adolescents are still growing, thus maintaining or slowing their weight gain can be very beneficial to their overall health. The generosity of the Sugar Ray Leonard Foundation supported the community weight management program by funding the salaries of two part-time community educators from January 2019 to September 2019.
To improve access to care for newly-diagnosed patients, the clinci developed and implemented group safety education classes.
In the past, newly-diagnosed patients needed to wait up to three weeks in order to be seen by physicians. With the implementation of the group safety classes, the wait time for patients diagnosed with T2D decreased to one week. The implementation of the group classes has also allowed us to see more patients—between January 1, 2019, and August 16, 2019, we have served 72 newly-diagnosed patients.
To facilitate the transition from pediatric to adult health care, the clinic created a transition-specific curriculum designed to empower patients to serve as their own advocates by speaking with their primary care providers about their diabetes.
Children’s Hospital Los Angeles offers specialized care to patients, particularly children and adolescents living with T2D. Most adults with T2D are treated by their primary care providers versus an endocrinologist, creating unique challenges for patients once they leave CHLA. Many primary care providers do not have experience managing the needs of such patients. In order to address this issue, we have created partnerships with two community health care clinics when our patients are ready to transfer from our care.
To provide comprehensive, coordinated care that better aligns with California Children’s Services (CCS) guidelines, the clinic hired a coordinator to identify the providers that each patient needs to see, manage the clinic flow and implement pre-clinic case conferences to ensure that all team members are aware of an individual patient’s needs and care plan.
The Sugar Ray Leonard Foundation’s grant supported the clinic coordinator’s salary from January 2019 to September 2019.
A HIPAA-compliant database was created to serve as a foundation for ongoing research in our T2D patient population and to evaluate the clinic model.
To date, the clinic has enrolled at least 230 patients in our database.
2014-2018 Highlights
Teen Power
Teen Power is an interdisciplinary intervention providing psychological support and skills-based learning for groups for adolescents ages 12-18 years with insulin-treated diabetes. Group sessions are also available for the teens’ caregivers and siblings. Caregiver meetings are conducted in English and Spanish.
Topics specifically address the emotional and behavioral barriers to optimal diabetes care such as communication, stress, depression, and diabetes burn-out. Dinner is provided which allows us to help with communications between teens and caregivers around the issue of food. We work with teens and families to develop/set goals for diabetes management behaviors and to promote effective adherence to these behaviors.
In 2016, funding from the Sugar Ray Leonard Foundation helped expand Teen Power's impact by sponsoring three new groups on CHLA's main campus or patients and families covered by commercial insurance. Two groups have been held to date, one starting in April and the other starting in July. Eleven teens with diabetes, joined by their parents and siblings, participated.
The many benefits teens and their families receive through Teen Power are evident by their direct expressions of thanks:
"Just a quick note to say how grateful I am for the work that you do. Teen Power was so great last night [My Son] said quietly to me when we got home, 'Thank you for taking me there, Dad'. I haven't pressed him on his experience, but he volunteered that he learned some really helpful things, and he seemed buoyed as we left. You will see us every week. Thank you."
"Thank you for such a great experience with the Teen Power group. All the kids, parents and leaders contributed to this experience in such a positive way. I feel [my daughter] has a better understanding and has taken steps to acknowledge her diabetes issues. Please keep us informed about any future Teen Power groups."
"I want to especially thank you for the past 10 weeks and I want to express how much I gained from our group meetings."
Kids N Fitness & KNF Junior
The Sugar Ray Leonard Foundation has supported the programs’ coordinators and instructors who lead a six-week course that focuses on nutrition education, physical activity and goal-setting for overweight children. Parents and guardians are also motivated to help their children by attending separate support groups during class time.
Since January 2013, 139 children ages 8 to 16 have participated in KNF and 56 children ages 3 to 7 have signed up for KNF Jr.
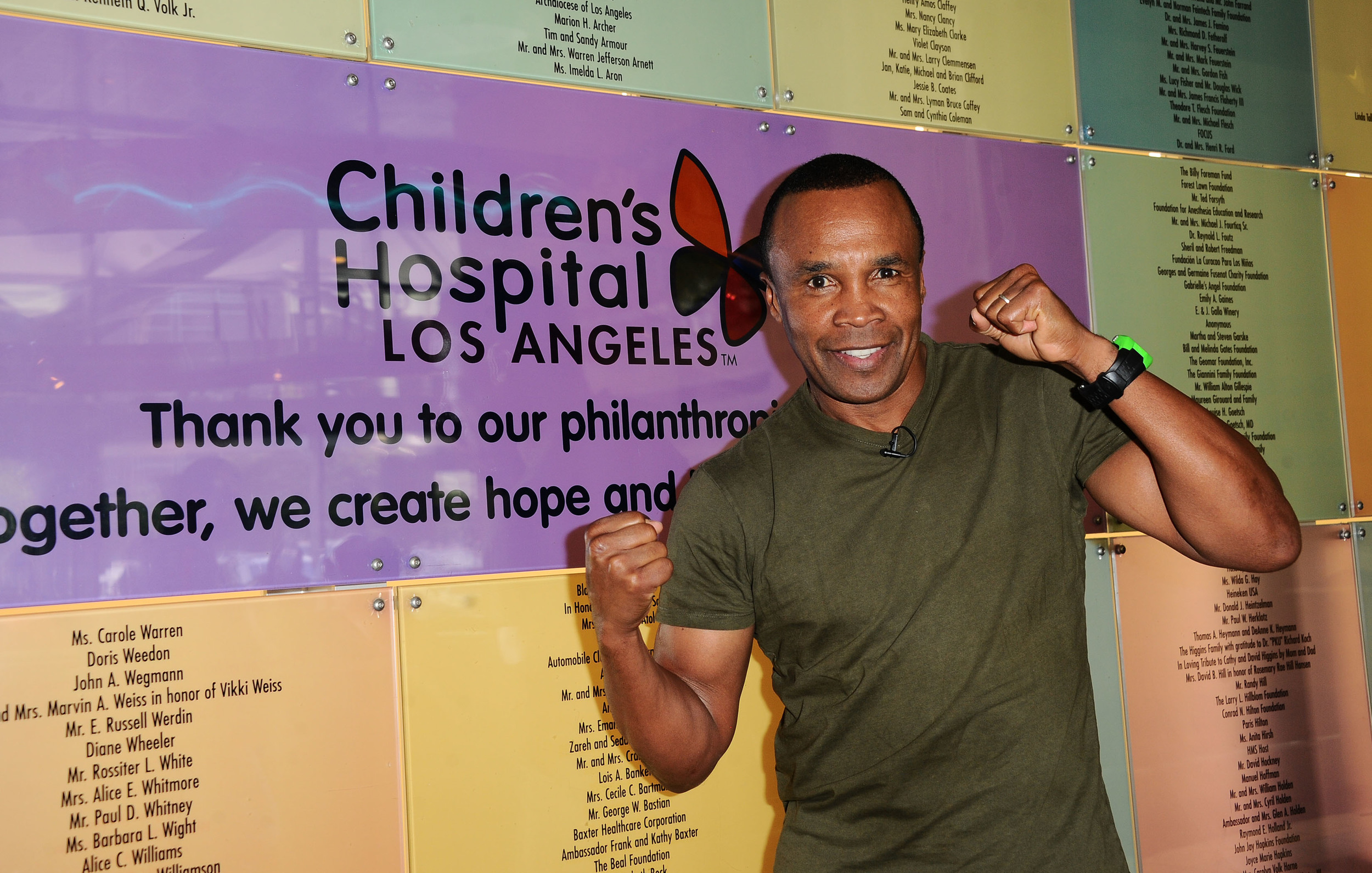
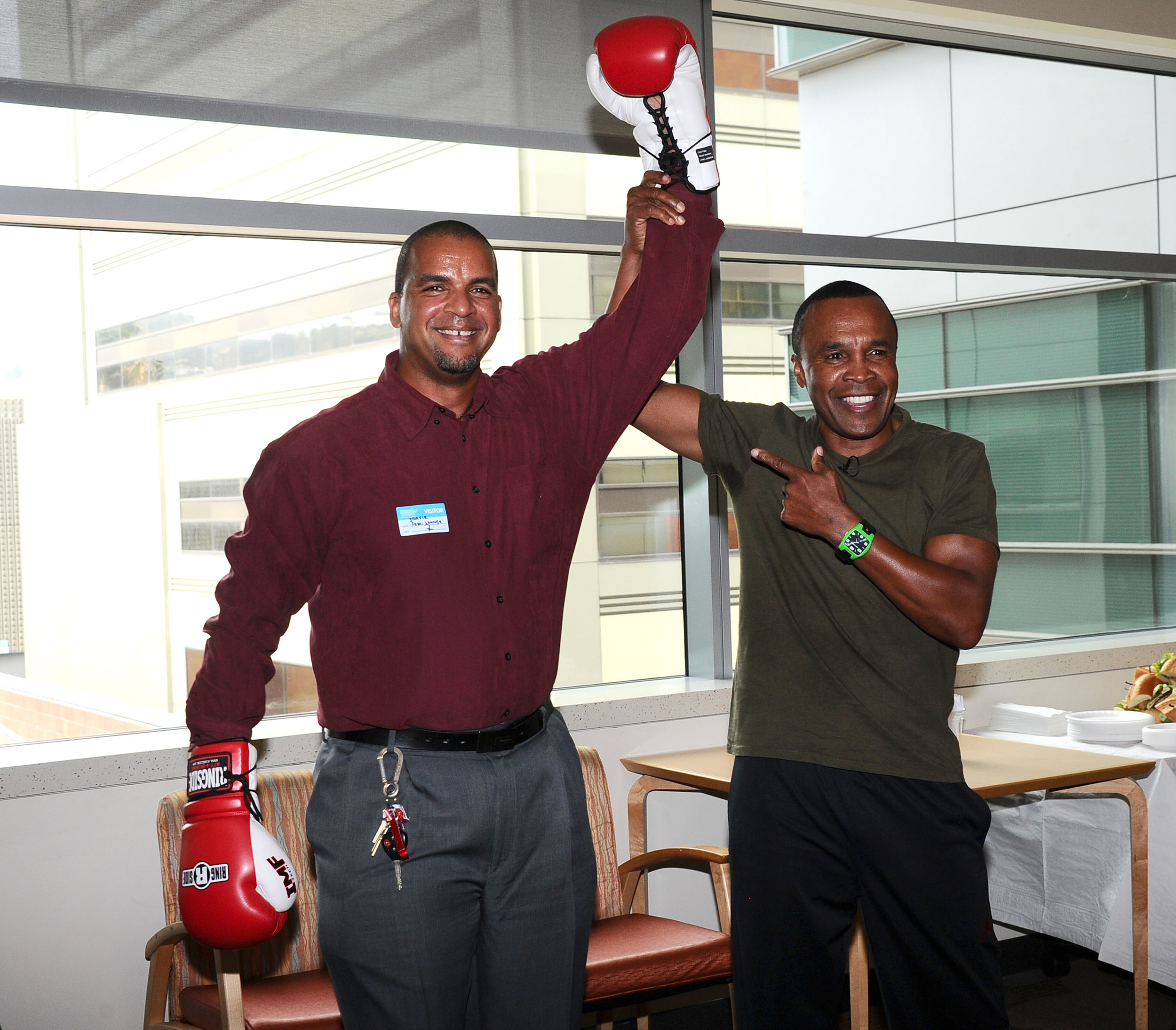
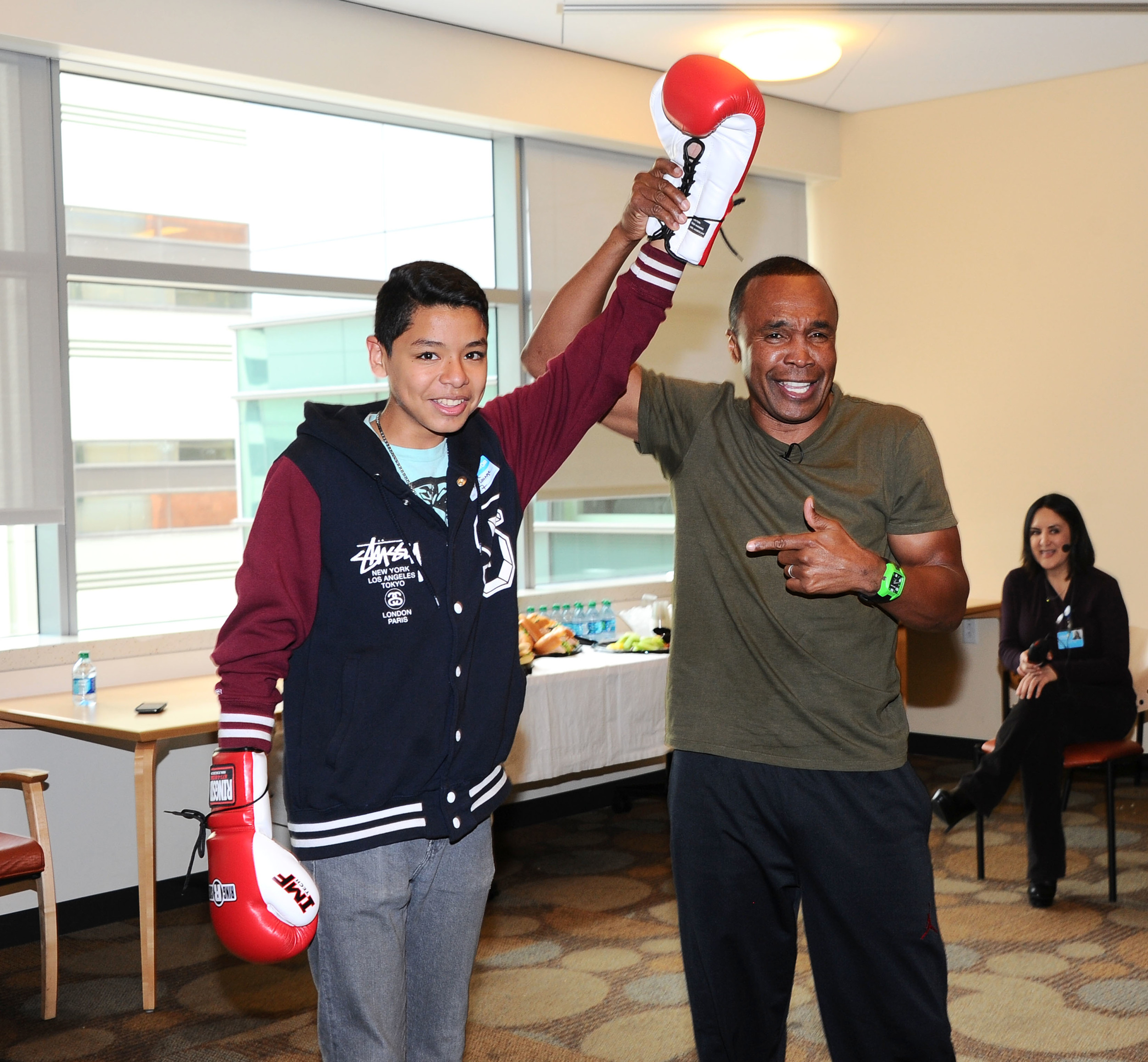
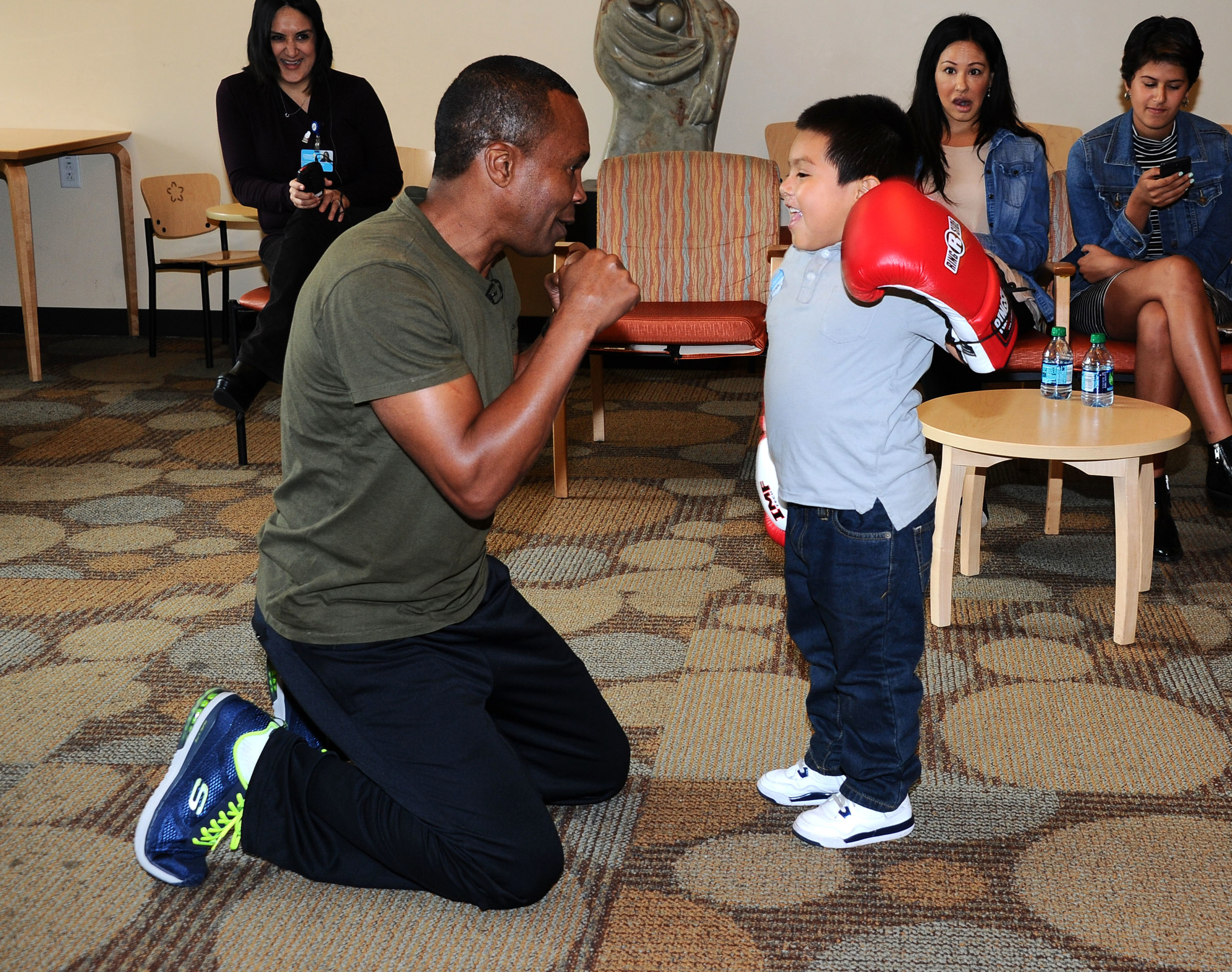
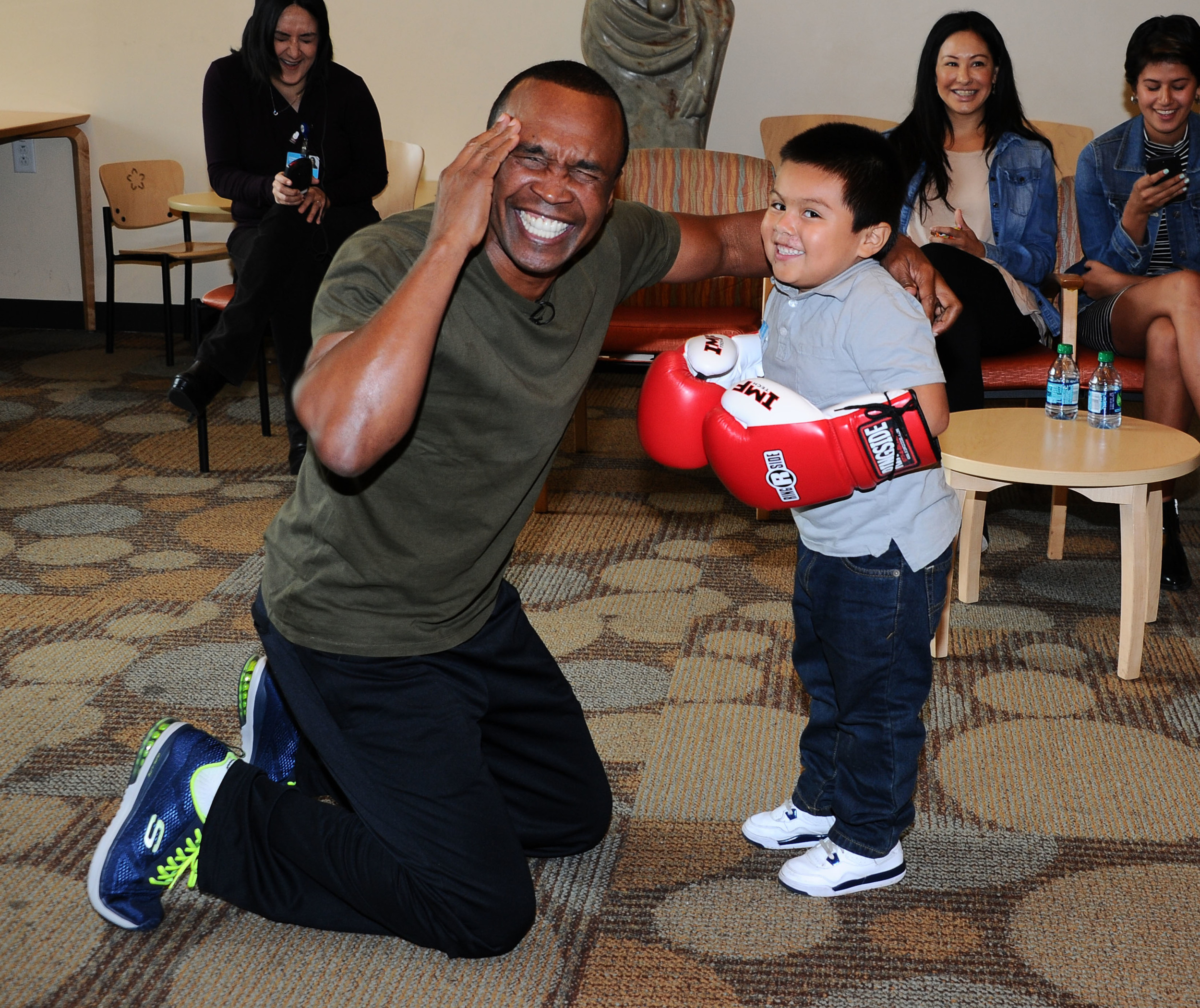
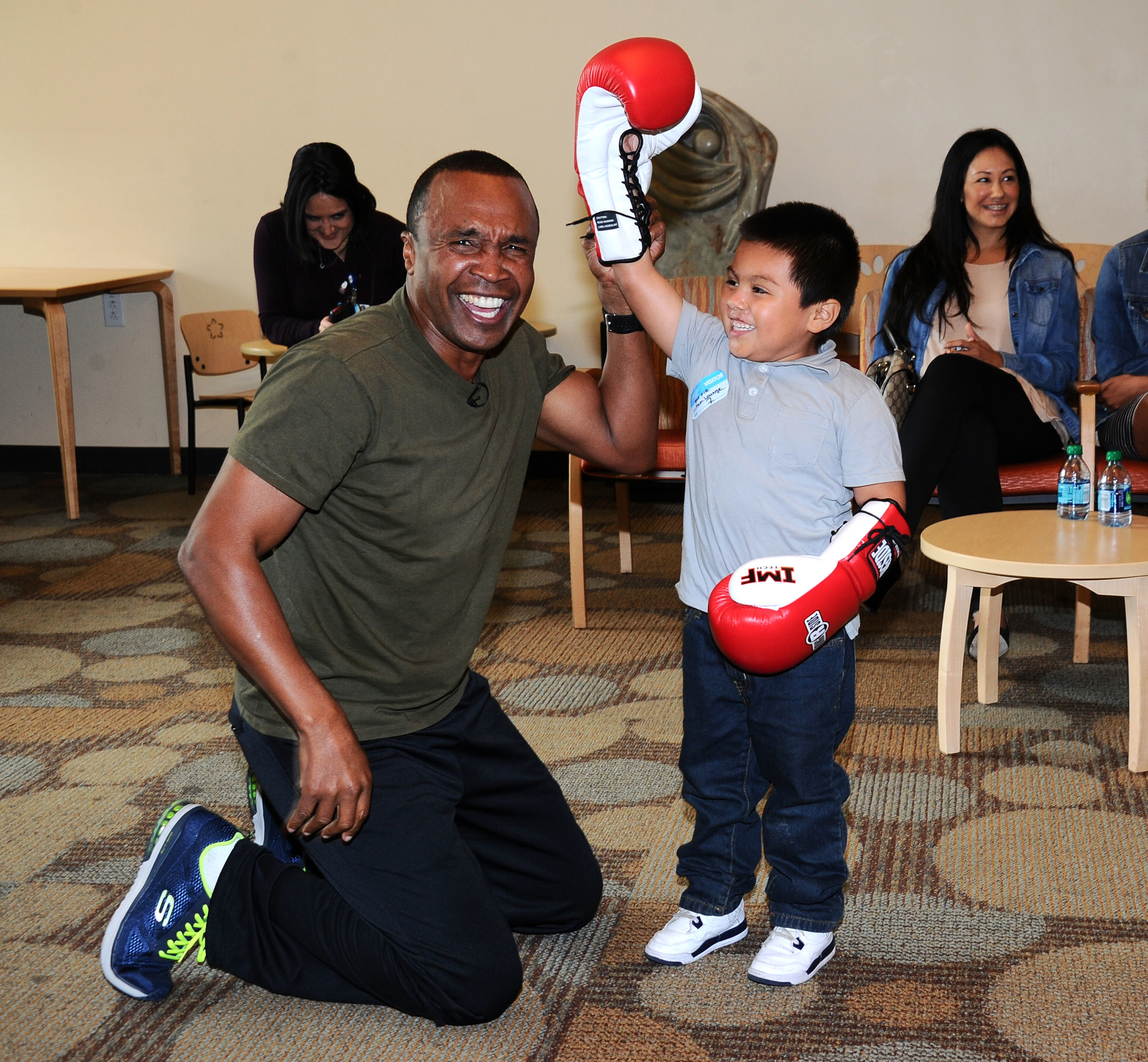
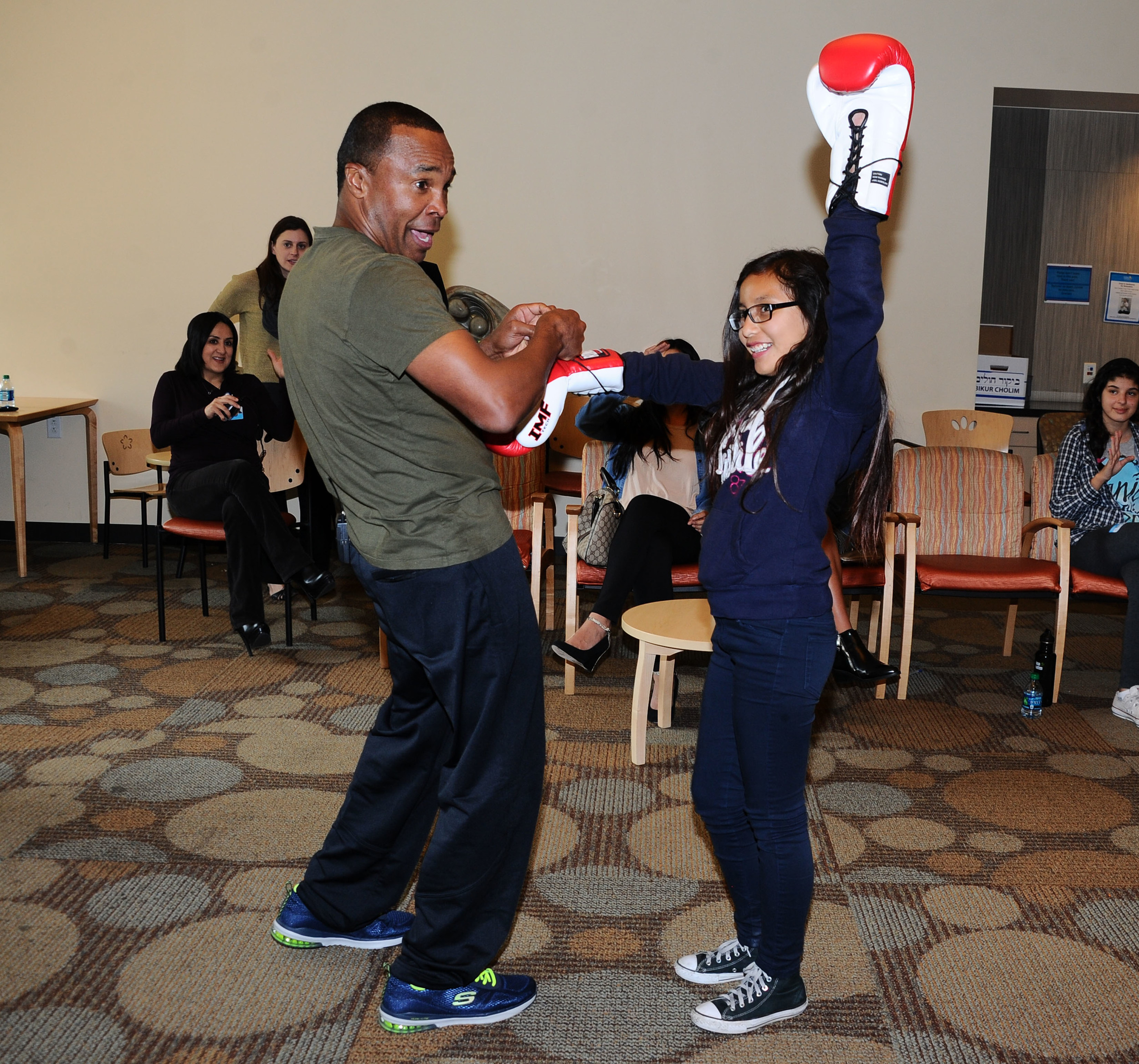
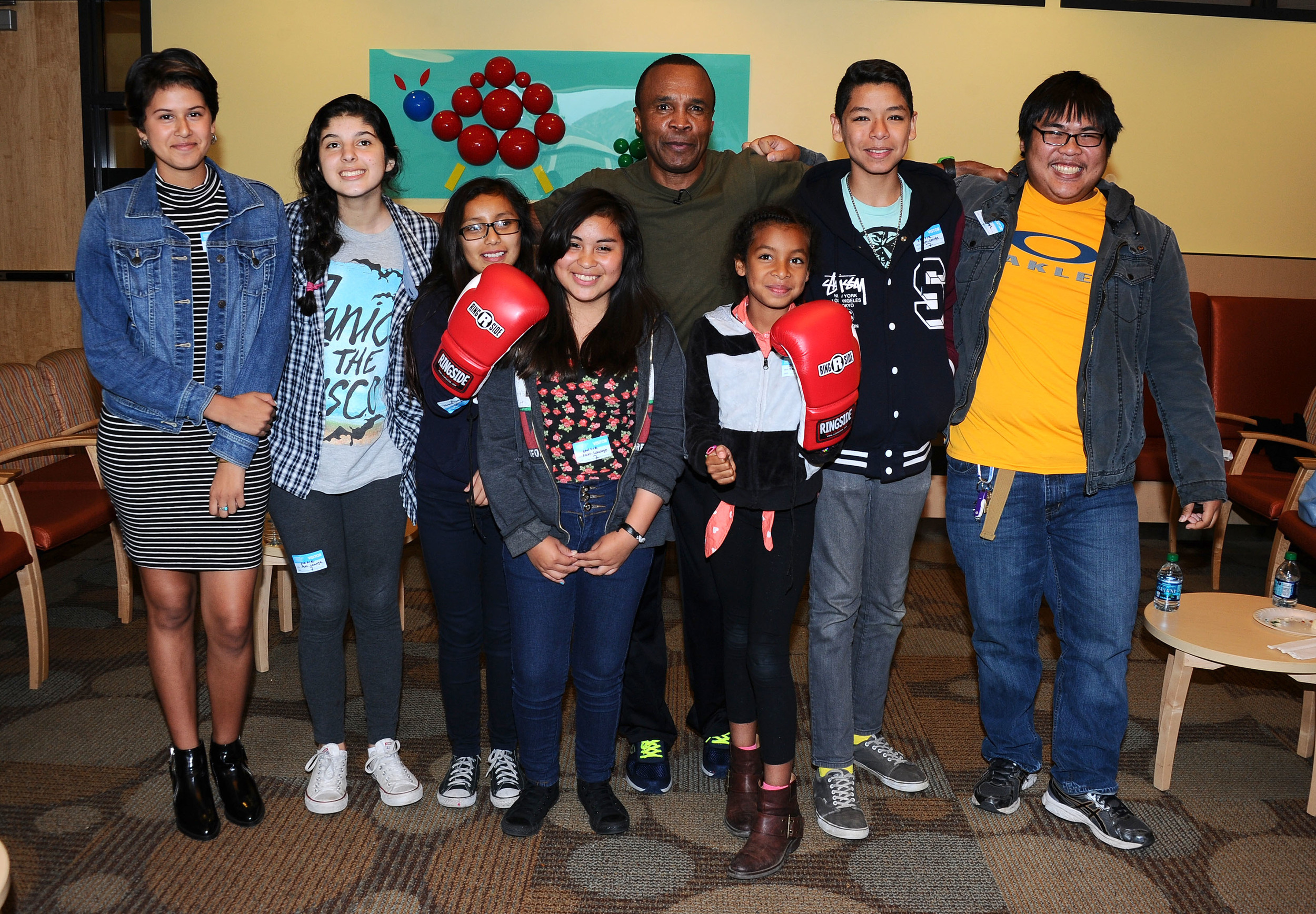
During a visit to the hospital, Sugar Ray filmed an informational video about “going toe-to-toe” with diabetes. It was posted on CHLA’s Facebook page and has been viewed more than 3,200 times.
HEAL Initiative
In November 2014, the Sugar Ray Leonard Foundation helped the Center mark the one-year anniversary of the HEAL (Healthy Environments and Active Living) Initiative.
The community-based project, which incorporates the KNF curriculum, was launched through a partnership with the New Mount Calvary Missionary Baptist Church. Speaking to a packed congregation at the South Los Angeles church, Sugar Ray spoke about the importance of healthy eating, exercise, and setting and reaching goals. By helping to deliver a positive message of fitness and well-being, our impact has been directional and motivational, inspiring children of all ages to set and reach their health goals.













More About Kids N Fitness©
Kids N Fitness© is an evidence-based, six-week weight management and healthy lifestyle program for overweight and obese children and their parents. The program was developed in 2000 by a multidisciplinary team from Children’s Hospital Los Angeles that included pediatric endocrinologists, dieticians, physical and occupational therapists, and social workers. The 1.5 hour weekly class consists of interactive nutrition education, physical activity and parent seminars. Kids N Fitness© is offered at CHLA and in low income community settings.
In 2009, The Sugar Ray Leonard Foundation began supporting Children’s Hospital Los Angeles and their Center for Endocrinology, Diabetes, & Metabolism. Because of the link between exercise, healthy diet and controlling Type 1 Diabetes and preventing Type 2, Sugar Ray Leonard was instantly drawn to this program. Leonard is passionate about health and fitness and hopes that he can inspire kids to lead healthier more productive lives through diet and exercise.
The Need
Currently over one third of our nation’s children and adolescents are clinically overweight or obese and nearly one third of low income preschool children ages 2-4 are overweight or obese. In 2003 the CDC Director Dr. Julie Gerberding stated that “…obesity is the number one health threat in the United States”. Obesity is also responsible for more than $190 billion in annual direct health care expenditures. Obesity is a multifaceted problem stemming from an imbalance in a complex regulatory system, and is affected by genetic, behavioral and environmental factors including social cues, easy access to inexpensive, high calorie food and drink (often of low nutritional quality), and lack of access to high quality food and opportunities to be physically active.
CHLA has found that Kids N Fitness© is especially effective when offered in a community setting such as churches, in local after-school programs, in schools, summer camps, and in community clinics. Their goal for the next 3 years is to train community educators and expand Kids N Fitness in South and East Los Angeles to make it accessible to families in greatest need.
Program Goals
Prevent and reduce the complications stemming from childhood obesity
Promote healthier eating habits, more frequent exercise, and a reduction in the behaviors that encourage weight gain
Provide support and motivation for families and provide them with the tools necessary to make better lifestyle choices that are sustainable
The Children’s Hospital staff is experienced in providing engaging lessons for the entire family. Families that participate in the program can look forward to:
Physical exercise classes
Interactive nutrition lessons
Understanding food labels
Healthy goal setting
Personalized feedback
Grocery store tour
A support system to guide behavior change
Healthy cooking tips
Fun weekly incentives
About Children’s Hospital Los Angeles
Founded in 1901, Children’s Hospital Los Angeles is the oldest freestanding children’s hospital in California. CHLA ranks among the top five in the nation on the U.S. News & World Report Honor Roll of children’s hospitals; it is one of only 10 children’s hospitals in the nation, and the only one on the West Coast, to make the prestigious list. The Hospital provides more than $221.4 million annually in community benefits to the children and families of Los Angeles.
The Center for Endocrinology, Diabetes and Metabolism at CHLA is at the forefront of patient care and research in diabetes, obesity, growth, bone, metabolism and endocrinology. It provides care to nearly 1950 children with diabetes and 5,100 children with other endocrine disorders.

